New Blood Signature Analysis May Help Diagnose Parkinson’s Disease Earlier
A new blood test may more accurately identify blood signatures, or biomarkers, for Parkinson’s disease (PD), according to a new study published in the journal Movement Disorders. The study, conducted by researchers at Mount Sinai and funded by the Michael J. Fox Foundation for Parkinson’s Research, applies a new approach to looking for blood biomarkers for both patients with and without a known genetic risk factor for PD. This paper is the fourth in a series that report new computational techniques to improve the identification of reliable blood biomarkers.
While biomarkers—such as bad cholesterol level in the case of heart disease—hasten diagnoses by offering accurate measures of disease progression, there are currently no fully validated biomarkers for PD.
The Mount Sinai study analyzed the blood of four groups of mice with genetic material (e.g. ribonucleic acids or RNA) predicted by researchers to form part of a PD signature. Researchers also examined the blood of a group of Ashkenazi Jewish patients living with PD, as well as a separate group of healthy controls. About half of the human subjects—both symptomatic PD patients and healthy controls—have small changes in their DNA code called mutations, in a gene known to increase the likelihood of developing Parkinson’s: leucine-rich repeat kinase 2, or LRRK2. Just one to two percent of Parkinson’s patients carry this gene mutation, and many LRRK2 mutation carriers are from the Ashkenazi Jewish population. The other samples studied came from individuals without the mutation, half of whom had clinical PD.
After comparing the mouse and human blood samples, researchers identified RNA signatures that can be measured in blood samples that correlate with the disease-causing mutations in the LRRK2 gene in PD patients.
While LRRK2 mutations contribute to PD risk in a small percentage of patients, researchers believe related pathways also play a role in much more common, non-inherited cases of PD. Studying it may speed progress toward treatments that would benefit everyone with the disease, not just those with genetic mutations.
“This is the first time we’ve studied animal models and clinical samples, and used them to look at RNA expression patterns of biomarkers in PD,” said Stuart Sealfon, MD, Chairman and Glickenhaus Professor, Department of Neurology, Mount Sinai Health System and lead author of the study. “Our other goal is to use this approach to identify subtypes of the disease so that treatment can be targeted more accurately and in addition, incorporated with clinical trials that facilitate the ability to identify new therapeutic and disease modifying agents.”
Parkinson’s disease (PD) is a chronic and progressive movement disorder affecting nearly one million people in the U.S. PD involves the malfunction and death of vital nerve cells in the brain, called neurons. Some of these dying neurons produce dopamine, a chemical that sends messages to the part of the brain that controls movement and coordination. As PD progresses, the amount of dopamine produced in the brain decreases, leaving a person unable to control movement normally. The cause of PD is unknown and there is presently no cure.
“The goal of this research is to improve early disease detection, especially in people who are carrying a predisposing genetic mutation,” said Dr. Sealfon. “If you can improve your ability to diagnose the disease more specifically and identify new subtypes, this can help overcome the hurdle in developing new treatments for Parkinson’s and other brain diseases. The next step is to replicate this approach in a larger sample, where we track patients longitudinally and see how profiles are changing over time.”
About the Mount Sinai Health System
Mount Sinai Health System is one of the largest academic medical systems in the New York metro area, with more than 43,000 employees working across eight hospitals, over 400 outpatient practices, nearly 300 labs, a school of nursing, and a leading school of medicine and graduate education. Mount Sinai advances health for all people, everywhere, by taking on the most complex health care challenges of our time — discovering and applying new scientific learning and knowledge; developing safer, more effective treatments; educating the next generation of medical leaders and innovators; and supporting local communities by delivering high-quality care to all who need it.
Through the integration of its hospitals, labs, and schools, Mount Sinai offers comprehensive health care solutions from birth through geriatrics, leveraging innovative approaches such as artificial intelligence and informatics while keeping patients’ medical and emotional needs at the center of all treatment. The Health System includes approximately 7,300 primary and specialty care physicians; 13 joint-venture outpatient surgery centers throughout the five boroughs of New York City, Westchester, Long Island, and Florida; and more than 30 affiliated community health centers. We are consistently ranked by U.S. News & World Report's Best Hospitals, receiving high "Honor Roll" status, and are highly ranked: No. 1 in Geriatrics and top 20 in Cardiology/Heart Surgery, Diabetes/Endocrinology, Gastroenterology/GI Surgery, Neurology/Neurosurgery, Orthopedics, Pulmonology/Lung Surgery, Rehabilitation, and Urology. New York Eye and Ear Infirmary of Mount Sinai is ranked No. 12 in Ophthalmology. U.S. News & World Report’s “Best Children’s Hospitals” ranks Mount Sinai Kravis Children's Hospital among the country’s best in several pediatric specialties.
For more information, visit https://www.mountsinai.org or find Mount Sinai on Facebook, Twitter and YouTube.
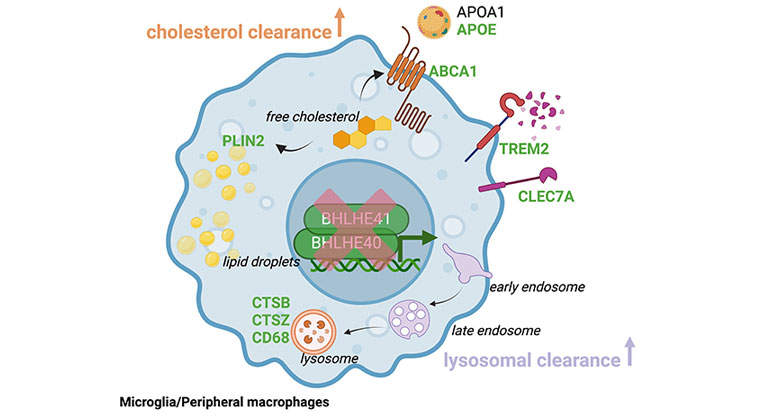
Immune Cells Identified as Key Players in Brain Health
Mar 21, 2024 View All Press Releases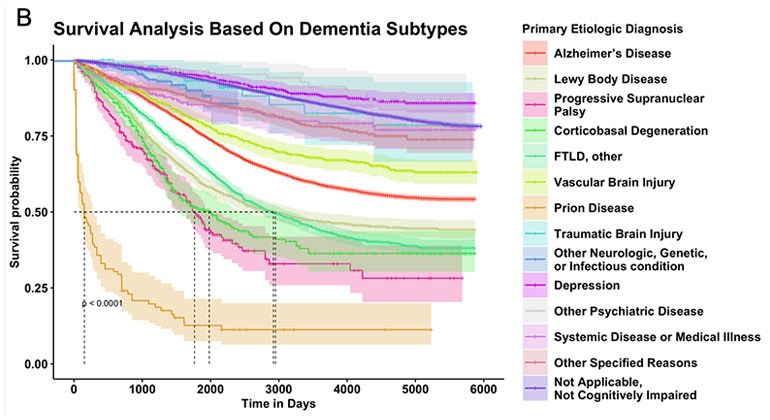
AI Finds Key Signs That Predict Patient Survival Across Dementia Types
Feb 28, 2024 View All Press Releases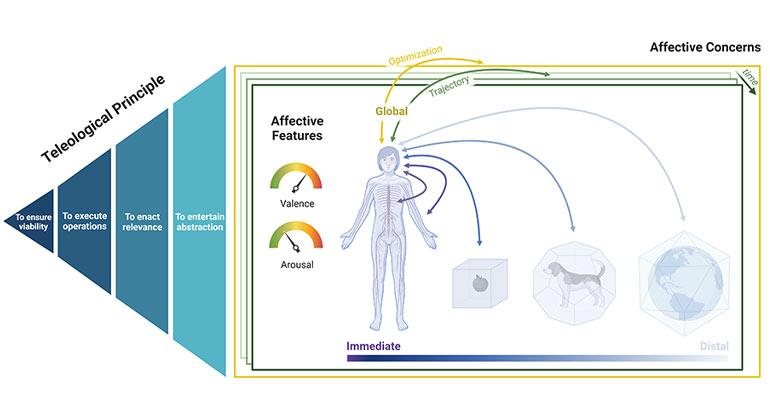
Global Taskforce of Scientists Develop a Unifying Framework for the Human Affectome
Feb 12, 2024 View All Press Releases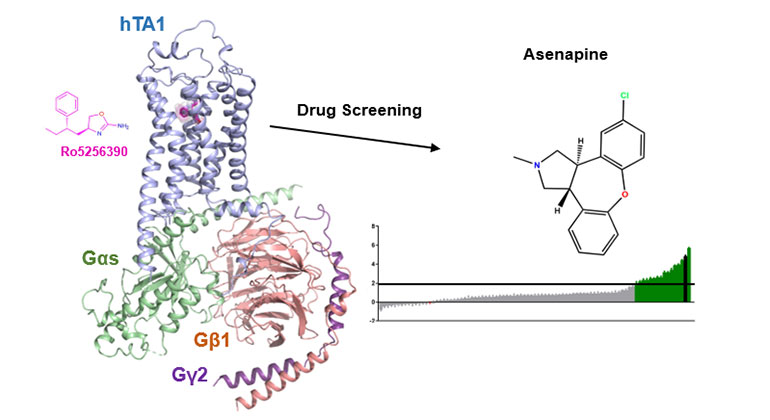
Demystifying a Key Receptor in Substance Use and Neuropsychiatric Disorders
Jan 02, 2024 View All Press Releases